Monday, March 30, 2020
Bring COVID-19 message to remote areas
By Pacharo Munthali
When the news broke out late last year of the novel Coronavirus, it sounded like a distance horror movie that may be gone before it finds its footing in the lands of Malawi. Just like Ebola and other corona family viruses, the thinking was that sooner than later, it would be gone. At least, so many thought.
Three months plus months down the lane, the footprints of the virus are becoming pronounced than ever. More than 30 000 people with cases of Covid-19 are gone. More worryingly more than 630 000 cases have been reported.
More countries are shutting down as the epidemic continues to wreak havoc. Health care systems have been pushed to the blink. While China has managed to recover, new ground zeros like Italy have emerged. There are fears for other countries too.
Coronavirus has continued to make its presence more conspicuous in more Africa countries than ever. While there have been few deaths within the continent, the number of confirmed cases is still on the rise.
Malawi like other African countries has been active. Steps have been taken to ensure that the country’s population is protected. While there are a number of approaches that have been put into practice, steps to ensure that people are in the know of the virus have been employed.
Switching on one’s local television and radio stations, it is clear to see and listen to jingles on COVID-19 being played. As one watches the jingles, the message is clear and constant – Wash your hands frequently; cover your mouth and nose with flexed elbow or tissue when coughing or sneezing; avoid close contact with anyone who has cold or flu-like symptoms; and seek medical care early if you or your child has a fever, cough or difficulty breathing.
Press statements and dissemination of information through social media especially Ministry of Health (MoH) Facebook Page coupled with continued media engagement has been clear.
During all this time the other constant occurrence has been consistent circulation of misinformation and rumours. The Ministry in one of its update says it has been “responding to rumours and misinformation to counteract” the vice that is liable to cause panic. Further, MoH says plans are underway to establish a toll-free line for inquiries (0887 37 12 88).
Actually there are so many myths. Others think the Covid-19 is not coming to Malawi. Some believe that if you circumcised then you cannot get the virus. Still there are other quarters that say if you have Group O you cannot get it. Some are saying Coronavirus is a natural occurrence the way it came is the way it will go. All these are some of the many misconceptions.
To deal with Covid-19, there is need for efforts from all stakeholders. The country has seen religious groups such as Catholic Church, Anglican, CCAP and Jehovah Witness – just a few – taking a lead in ensuring that members of their respective groupings and communities at large are in the know. This is the disease that may be detected during one of the tests, or may never be found in Malawi. But knowing its symptoms and how to avoid it is paramount.
More still needs to be done.
While Malawi government is currently using traditional media and new media to ensure that as many people as possible are in the know of Covid-19, there is need for more efforts aimed at penetrating to the hard to reach areas.
As a country, we have always lived a life of togetherness, a kind of approach that may not be in tandem with what is being preached – to curb the spread of Corona virus, people are being advised to maintain social distance. Now we are in a society where maintaining social distance has never been part of our narrative. As a country how are we planning and coming up with communication approaches that will provide an ideal platform that will make people understand this reasoning? While toll-free is important, at this infant period here in Malawi it would be great to employ community based communication approaches that understand the ecological side of people.
On Health Promotion part, apart from using approaches like the ones that Ben Mankhamba using a public address system has been helping communities to understand more about the the virus. In addition to HSAs, empowering community based structures including faith based structures that have already started playing their role with right information it will be important for the whole population to be in the know.
In Health Communication, employing a number of approaches with the same message but for the different audience is important. To have a gratifying uptake of the message it is important to segment the audience.
An informed citizenry means empowerment. People will be able to know what is right or wrong. The anxiety that comes with fake news and rumours will be dealt with.
As the World Health Organization (WHO) warned a week ago - the window of opportunity to prepare is closing and that critical gaps remain.
"Every country can still change the course of this pandemic by scaling up their emergency preparedness or response," said Matshidiso Moeti, the WHO's regional director for Africa quoted by the BBC.
The Author is Development Communication and Community Engagement Scholar, writing in his personal capacity.
Monday, August 5, 2019
Stopping Aids before it kills
James Chavula July 20, 2019 0 Comments
It is 11.20am when we venture into the snaky corridors of Nsanje District Hospital, formerly a refugee camp for Mozambicans who fled civil war in the 1970s.
It is sweltering in the border district’s largest health facility, where a tuberculosis patient concealed as Moira is readmitted to the emergency bay of a newly refurbished female ward.
Moira undergoing treatment at Nsanje District Hospital
The 36-year-old is one of nearly 400 patients with advanced HIV treated at the facility since she was first admitted in January. Some health workers fear the count may exceed the 500 treated between July 1 2017 and December 31 2018. To them, the caseload exposes a gap in the national agenda to end Aids-related deaths.
‘I’ve gone through a lot’
Long-serving staff remembers an era of mourning—2006 to 2017—when about a third of inpatients with conditions related to HIV were dying amid lengthy delays in diagnosis and treatment of advanced HIV. The condition is usually characterised by deadly opportunistic diseases that get worse as immunity falls, evoking images from the turn of the millennium when Aids was terminating five times the lives it claims nowadays.
Calls for community inroads: Likaka
The sights have become sporadic since the country liberalised access to antiretroviral (ARVs) in 2005. National Aids Commission (NAC) reports that free ARVs for all have slashed Aids-related deaths from 64 200 to 13 000 in the past 15 years.
UNAids estimates show nearly 17 000 people with HIV die every year.
However, Moira’s debilitating loss of weight personifies lapses in ensuring every HIV positive person takes life-prolonging drugs consistently until the virus becomes undetectable and unlikely to be transmitted.
“I’ve gone through a lot,” she states. “I was forced to taking the drugs because I could go a day or so without food. I couldn’t take the drugs on a flat stomach. One needs adequate nutritious food for the drugs to work.”
When she was diagnosed with TB at Bangula Health Centre, the mother-of-three and her family were among 3.3 millions Malawians in need of urgent food aid following severe drought and pest attacks.
She explains: “I was sickly and frail. By August, I started experiencing chest pains, coughing out thick stuff and perspiring at night.
“A clinician at Phokera Health Centre referred me to Bangula, where they further referred me to Queen Elizabeth Central Hospital (Qech) in Blantyre after they detected advanced TB.”
Easily forgotten
Moira first arrived at Nsanje District Hospital six months ago on return from the Southern Region’s largest referral hospital. Her three sisters have been taking turns to ensure she receives adequate care.
“After taking the TB drugs, she briefly got better. However, coughing recurred and her face started swelling. We rushed to Qech for tests, got some new drugs and came straight here,” says Maria Medisoni, her guardian.
The long travels and hospital stays worsen poverty among people with HIV and their guardians. Bringing vital services closer to where they live lessens their financial hardship in fulfillment of the universal health coverage (UHC) policy.
Dr Andrew Likaka, director of quality management and UHC in the Ministry of Health, urges government and its partners to invest more in community-level initiatives to improve quality of care of patients with HIV even in hard-to-reach areas.
He states: “Being at the tail end of the country, it is very easy for border districts such as Nsanje to be forgotten even though this is where the best results and impacts are happening.
“It puzzles me that more donors concentrate on the capital, Lilongwe, and surrounding areas. If you tell them to extend their programmes to Nsanje, they think twice.”
He reckons Malawi has made a tremendous progress in the global push to ensure 90 percent of all people living with HIV know their status, 90 percent of all diagnosed with HIV are put on treatment and 90 percent of all people on ARVs achieve suppressed viral load.
Closing the gaps
At the United Nations, UNAids’ dashboard of the country’s progress towards 90-90-90 goals shows that an astonishing 91 percent know their status, 83 of those diagnosed with HIV started taking ARVs and 90 percent of them have undetectable viral load.
But the refurbished ward Moira occupies was a dilapidated monument of neglect just three years ago. Patients were often stretchered into the ward after enduring a long search for accurate diagnosis and treatment for opportunistic infections. Medcins Sans Frontiers (MSF-Belgium) bankrolled the rehabilitation of the ward and the installation of the rapid assessment unit at the hospital.
Despite this progress, HIV remains the leading killer among adults—causing nearly 17 000 deaths a year.
According to the world Health Organisation (WHO), the decrease in Aids-related deaths has stagnated.
Still, many patients are at risk of being left behind in national efforts to end Aids-related deaths, including the universal access to ARVs.
MSF country representative Ilse Casteels says the country needs to intensify efforts to end deaths from conditions catalysed by advanced HIV.
“Despite the impressive strides, challenges remain as 21.7 percent of HIV patients still don’t know their status and a significant number of patients has interrupted their treatment and are lost to follow up. Other patients are failing on treatment, but only low proportion of them has been switched to the second line ARV,” she explains.
In Nsanje, MSF is working closely with the district health office to improve the circle of care.
They have deployed community health promoters who sensitise patients to swiftly seek medical assistance when they sense danger signs. They have also equipped health centres to screen patients for infection associated with dwindling immunity.
“If necessary, the patients are referred to the hospital,” says Brains Kamanula, one of the counselors credited with inroads to stop advanced HIV at community level.
When patients and guardians arrive at Nsanje District Hospital, Kamanula chats with them to assess “red flags”. For Moira and her colleagues, the initial patient assessment involves ticking a checklist.
He explains: “When we met, she ticked all the boxes when it comes to knowledge about HIV and how to take ARVs, but her nutrition was not OK. She was receiving minimal care and support.
“Being financially constrained, the husband was usually away from home, doing piecework to source food and other basic needs,” he explained. Unfortunately, she was lost to follow up because the family has no phone,”
Kamanula and his fellow community health promoters conduct community outreach meetings and door-to-door visits to publicise the importance of taking ARVs without fail and going to hospital when the sense danger signs.
“If a patient adheres to drugs, the virus is suppressed and the immunity improves, so one can be healthy like any other person. In her case, she presented late with TB. That’s why we referred her to QECH,” he explains.
Left behind
However, some people are not reaping the benefits of the country’s test-and-treat because they either interrupted antiretroviral treatment or they take drugs intermittently.
Apart from nutritional gaps, some people living with HIV are forced to quit treatment by faith healers who misconstrue suppressed viral load and restored immunity for cure.
A man diagnosed with HIV at Ndamera Health Centre on the border between Malawi and Mozambique seven years ago bemoaned long trips to replenish the drugs, saying it can be costly for poor families.
He started taking ARVs when a daily dose entailed a handful of tablets per day. Now, one takes just a pill day, with the Ministry of Health already planning to introduce a fast-acting pill by January 2020.
NAC spokesperson Karen Msiska credits the current pill for reducing default rates and improving the outcome of the new strategy of ensuring everyone diagnosed with the virus is put on treatment immediately.
“Currently, the default rate in the country is
[estimated]
at less than two percent. This includes those who transfer from one centre to another without proper documentation, deaths that are not properly documented as well as those who literally stop ARVs,” he says.
However, the drop-out rate is much higher in some districts, including Ntcheu, where district ART coordinator Davie Muhasuwa recently reported that nearly 40 percent of those on treatment can no longer be traced.
This increases the likelihood of advanced HIV and slows the pace towards achieving the 90-90-90 goal to combat Aids.
“ARVs help reduce the spread and impact of HIV in communities, so it is disheartening that some patients are defaulting. This is a setback towards the attainment of the HIV initiative,” says Lyness Soko, Malawi Network of People Living with HIV (Manet+) resource mobilisation and advocacy officer.
A long way to go
Besides raising mass awareness to stop HIV-related conditions before they get out of hand, MSF has embarked on a mentorship programme in some sites to improve the competences of the clinical staff.
Nsanje district medical officer Dr Alfonsina Ndembera put the interventions in context: “The mentorship programme and rapid assessment unit integrated into our emergency unit has improved our capacity to promptly diagnose patients with advanced HIV and put them on treatment.
“Most of patients arrive in a critical state, often with a host of infections that we have to treat before we put them back on a second line of ARVs. Treatment is nothing unless we can accurately detect their illnesses.”
She thanks MSF for refurbishing the ward and training its medical staff to improve the conditions in which the patients are hospitalised.
Looking back, Casteels says she felt relieved when she received a proposal to divert funding for patients nutrition towards giving the ward a new look.
Three years ago, the oddities in Moira’s ward included dirt falling off a roof with ceiling boards missing, holes in the walls, broken windows, insects crawling under the beds, dusty floors as well as toilets and showers patients feared to step in.
“Despite the improvements made, there is still a long way to go. The district is still confronted with important human resource gaps, with lack of essential medication/and equipment.”
Tuesday, April 16, 2019
The villages in Malawi that prepared for the floods - and survived
29 March 2019
In the heavy rains that preceded Cyclone Idai, a broad swathe of southern Malawi was submerged by flood waters. At least 60 people have died, and tens of thousands were made homeless. But things could have been much, much worse. Understanding how affected communities took steps to protect themselves, sometimes long before the waters rose, is key to understanding how to mitigate the impact of extreme weather events in the future. In the stories of these villages lie the lessons that southern Africa must learn if it is to have any chance of coping with climate change.
By Simon Allison in Ndamera and Chikali
On March 8, in the late evening,
Edward Biasi was at home listening to the radio. It was still raining,
like it had been for the last week. The news was alarming:
meteorologists were predicting even more rain, and possibly floods.
With the luxury of hindsight, we know that Biasi was in the middle of the heavy storm that would leave much of southern Malawi underwater. The storm then headed out into the Indian Ocean, where it gathered energy, returning as Cyclone Idai to pulverise Beira and surrounding provinces in both Mozambique and Zimbabwe.
![]() But Biasi, a portly old man with
an absence where his front teeth should be, did not have the luxury of
hindsight. He is the Group Village Headman for Thaundi, a small,
picturesque village on the west bank of the Shire River, population 330.
It is in the heart of the southern wetlands, a vast plain of arable
land ringed by mountains. In the good times, the topography makes this
the most fertile soil in the country. “You don’t need fertiliser,
everything just grows,” said Biasi. In the bad times, the plains act
like a giant bucket, collecting all the water that runs off the hills.
But Biasi, a portly old man with
an absence where his front teeth should be, did not have the luxury of
hindsight. He is the Group Village Headman for Thaundi, a small,
picturesque village on the west bank of the Shire River, population 330.
It is in the heart of the southern wetlands, a vast plain of arable
land ringed by mountains. In the good times, the topography makes this
the most fertile soil in the country. “You don’t need fertiliser,
everything just grows,” said Biasi. In the bad times, the plains act
like a giant bucket, collecting all the water that runs off the hills.
Among Biasi’s many responsibilities is reacting to extreme weather warnings. Knowing how to respond is never easy. Evacuating means abandoning the maize and bean crops, which were weeks away from harvest, and this year was on track to be a good one. Without that food, the village cannot eat. It also means leaving livestock to their certain deaths.
Nonetheless, he made his decision quickly. Bitter experience has taught him the value of caution. It was time to pack up and go.
This is not the first time he has had to make such a difficult call. Biasi has been headman since 1978, when he took over from his grandfather. He cannot remember how many times Thaundi has had to be evacuated, but he does know that it is happening far more often than before. The last major flood in southern Malawi was just four years ago, in 2015, in which at least 176 people were killed. “In my village we always get flooded. But it’s different from the past. It would happen once every ten years, and the waters weren’t so high. Now it’s more frequent.”
After each disaster, with increasing reluctance, he returns home. “We keep going back because we can’t have land anywhere else.”
Five chiefs report to Biasi, and at around 10pm he spoke with them about the impending disaster. They did not have a formal, sit-down discussion - there simply wasn’t time. Preparations to leave began immediately, and by 8am the next morning the first canoes were crossing the river, heading to the relative safety of Ndamera, a larger village on higher ground on the other side of the river. Ndamera has for decades offered refuge when the waters come.
There was no room for people to bring much in the way of belongings - just the clothes on their backs and maybe a few pots and pans - and all the goats, chickens, and guinea fowl had to be left behind.
Not everybody heeded the call to evacuate. “Most left, but some stayed,” said Biasi. “Sometimes people are not sure, they think the water is not moving so fast. But this time they were wrong.”
Never a bluegum
In times of great calamity, the smallest details can be the difference between life and death. What saved Nessie and her family’s life was the knowledge that bluegum trees become slippery when wet. Mango trees, however, retain their grip.
![]() Nessie, 35, along with her husband
and two children, had decided to remain in Thaundi, hoping and praying
that the waters would not rise any further and that they would not have
to abandon their whole lives and start again from nothing. The prayers
were in vain. A night or two after the rest of the village had left -
she cannot remember exactly when - she awoke to the feeling of moisture
on her face. She rose quickly, and stepped outside. The river had
spilled its banks, and the water was up to her knees. She quickly woke
the family.
Nessie, 35, along with her husband
and two children, had decided to remain in Thaundi, hoping and praying
that the waters would not rise any further and that they would not have
to abandon their whole lives and start again from nothing. The prayers
were in vain. A night or two after the rest of the village had left -
she cannot remember exactly when - she awoke to the feeling of moisture
on her face. She rose quickly, and stepped outside. The river had
spilled its banks, and the water was up to her knees. She quickly woke
the family.
She strapped her two-year-old daughter to her back with a fold of chitenge. Her husband took their seven-year-old son. They looked for a suitable mango tree - never a bluegum - and clambered up.
And then they waited, watching as the water rose until their house and all their belongings were totally submerged. For two long days and longer nights they waited, but no one came to their rescue. While she waited, Nessie could not stop thinking about what happened to another woman in her village, in the 2015 floods. This woman, also stuck in the high branches of a tree, collapsed with exhaustion and fell into the water below. Neither her nor her baby survived. Even now, with Nessie’s baby giggling safely on dry land, this is all she can think about. “I keep imagining what would happen if I fell into the water and what would happen then.”
She didn’t get much sleep on the tree. “There were times when I dozed off, but I would wake up every few minutes. We were so hungry. The baby was so hungry that she was biting my arm.” Eventually, a fisherman rowed up in a dugout canoe, searching for survivors. Rescue came at a price - 1000 Kwacha (R20) per person - but the family was in no position to bargain.
The fisherman rowed them to a makeshift port on the east bank of the river, where they waited for another two days with no blankets or mosquito nets, and only a few handfuls of food, until word came from their chief to join the rest of the village in Ndamera. “This time, it’s better than in 2015. This time no one from our village died,” said Nessie.
Even my laugh is weak
Joel Kadalinga, 47, saw trouble coming - years ago. After the 2015 floods, he saved up to build a house in Ndamera. “Our area is a flood and famine area. One year I got the money and I moved. It’s very safe here because it’s up.” Him and his family still live and farm in Thaundi. They grow maize to eat, and beans and sugar cane to sell. But at the first hint of floods to come, they escape to Ndamera, only a couple of hours away in normal times, to wait it out. This year they moved in January, just in case, and when the river began to rise in Thaundi they were already in a fully-equipped place of safety.
“It was hard for the village to sense that this was a dangerous situation,” he said. “The weather these days is unpredictable. It was only when the water was up to their necks that they moved.”
![]() Kadalinga was on hand to welcome
the villagers displaced from Thaundi when they straggled in, as well as
those from dozens of other villages who made there way here. There are
4747 displaced people in Ndamera, from 1150 households. He has taken on a
formal role as camp secretary, helping to manage the allocation of food
aid and to oversee the various water and sanitation projects that aid
organisations are implementing. For example, Unicef, the United Nations
children’s agency, has built a water treatment plant to filter the
contaminated borehole, and installed several new toilets.
Kadalinga was on hand to welcome
the villagers displaced from Thaundi when they straggled in, as well as
those from dozens of other villages who made there way here. There are
4747 displaced people in Ndamera, from 1150 households. He has taken on a
formal role as camp secretary, helping to manage the allocation of food
aid and to oversee the various water and sanitation projects that aid
organisations are implementing. For example, Unicef, the United Nations
children’s agency, has built a water treatment plant to filter the
contaminated borehole, and installed several new toilets.
There is only so much anyone can do, however. Although all the new arrivals have some form of temporary accommodation and the children have been welcomed into the local school, food remains scarce. Rations provided by government and humanitarian agencies are just two cups of maize meal per family per day. For the rest of their diet, the men go out to hunt or fish or forage, or try to pick up piece work in unaffected communities. It is never enough. “I’m so hungry that even my laugh is weak,” said Nessie.
Kadalinga is even more worried about what happens when the flood waters recede, and the villagers of Thaundi return home. “Three months from now, we will go back. We will continue with our yearly activities. All the moisture in the soil means that the next harvest will be excellent, but we have to survive until then. We need support to do so.” And then? “We are worried. It’s tiresome. We build our homes and then two or three years later they are destroyed.”
For Biasi, the Thaundi headman, there is no small measure of pride that he made the right decision. Despite the devastation of their homes, no one from Thaundi died in the floods. No one was injured. But he knows, if the weather continues to behave so erratically, that there will be a next time. “I don’t think the village will still be there in 50 years. I don’t think anyone should live there now. But that’s the only land that we have, so what choice have we got? It’s very painful for me and my people, but we have no choice.”
Thaundi is not the only village to notice the
new weather extremes. All across the southern Malawi wetlands,
communities are making plans to deal with what is swiftly becoming the
new normal.
In Chikali village, also on the west bank of the Shire River, very near the border with Mozambique, memories of the last great flood are fresh. It was only four years ago, in 2015, and ten people from the village were killed. Markson Beka remembers it well: the waters rose at night, and it was chaos as people ran around in panic, not knowing what to do or where to go.
This time, when the floods came, the village reacted totally differently. Despite 1799 households in Chikali and the surrounding area being affected, there were no casualties. Not one. “It’s because of the awareness we created. We told people to move in time. We had a plan,” said Beka.
![]() Beka is the chairperson of the
area’s Village Civil Protection Committee, a body established by the
government in 2009. The committee is composed of representatives from 45
nearby villages, and receives irregular disaster-management training
from the government.
Beka is the chairperson of the
area’s Village Civil Protection Committee, a body established by the
government in 2009. The committee is composed of representatives from 45
nearby villages, and receives irregular disaster-management training
from the government.
The committee learned from the mistakes made in 2015, and put in place procedures to prepare for the next disaster, and to mitigate its impact.
The first step was to train residents to recognise the warning signs. “When we see more ants, that is a sign that more rains are coming. When we have continuous days of rain, then we can expect a flood,” said Beka.
Next the committee created assembly points on higher ground, so that people would know exactly where to go when they sensed trouble. This is not an option for all villages, but Chikali is lucky in that it is relatively hilly, and some areas are safe from floods.
The committee toured around all the low-lying settlements to ensure that everyone knew what to do when disaster struck.
![]() When the floods did come, the response
was calm and orderly. Brains Kamanula, a 54-year-old community health
worker with Doctors Without Borders (MSF) who lived through the 2015
floods, said that the committee’s meticulous preparations made all the
difference. “When the water came, they [community leaders] could not
allow people to run around. They said come together in a single point
and they looked where the water is going. They had whistles. Some
climbed into a tree to check the direction of the water.”
When the floods did come, the response
was calm and orderly. Brains Kamanula, a 54-year-old community health
worker with Doctors Without Borders (MSF) who lived through the 2015
floods, said that the committee’s meticulous preparations made all the
difference. “When the water came, they [community leaders] could not
allow people to run around. They said come together in a single point
and they looked where the water is going. They had whistles. Some
climbed into a tree to check the direction of the water.”
The significance of the whistles cannot be overstated, he said. Not only does the whistle serve as an alarm bell, it also allowed committee members to easily direct nervous crowds to places of safety. Again, in an emergency, it is the smallest details that can make the difference between life and death.
![]() “The communities are prepared. The
government implemented the village civil protection committees, which
are very important. In each village, there is one or two members. Their
preparedness for disaster is better because they were trained. The
community has points that have already been chosen and everybody knows
where to go.”
“The communities are prepared. The
government implemented the village civil protection committees, which
are very important. In each village, there is one or two members. Their
preparedness for disaster is better because they were trained. The
community has points that have already been chosen and everybody knows
where to go.”
Enelisi Wiseman was among those affected. When the whistles sounded, her and her family knew what to do. “When the disaster happened we were in our village. We then moved into the primary school.” Several days later, the village headman allocated land for her and 114 other households to construct temporary accommodation while they wait for the flood waters to recede. The new accommodation is already being built: reed huts to replace the clay-brick houses.
Around the village, at least in the areas where the waters have receded, the ruins of the houses that were destroyed are obvious in the collapsed walls and the piles of tumbled-down bricks; and in the patches of bare earth where even foundation stones were ripped from the ground.
![]() The first thing Wiseman’s
displaced community did was to construct two temporary toilets, one for
men and one for women and children. When Kamanula arrived on the scene,
and saw what they had built, he could not contain his pride. “All the
awareness on hygiene and sanitation that MSF has been doing, it is
really working,” he said.
The first thing Wiseman’s
displaced community did was to construct two temporary toilets, one for
men and one for women and children. When Kamanula arrived on the scene,
and saw what they had built, he could not contain his pride. “All the
awareness on hygiene and sanitation that MSF has been doing, it is
really working,” he said.
Food remains a problem, however. The area is accessible only by boat, which makes it hard for humanitarian organisations to get there. Everyone’s crops have been decimated by the storms and the floods, and what little is left is being strictly rationed.
It could be several months until Wiseman and her family return home. When they gets there she will have to start again from scratch. She knows that hers is not a sustainable lifestyle in the long-term, that something has to change. “We have a tentative solution that we have discussed amongst ourselves,” she said. “We are desperate so we will go back and build temporary houses and go and plant our crops. After we harvest, we will go and ask the chief if we can have some land somewhere higher up.” This time she escaped with her life, and she doesn’t want to have to do it again.
(Photographs: Simon Allison)
http://atavist.mg.co.za/the-malawian-villages-that-took-on-the-floods-and-survived?fbclid=IwAR1kLik0FdDfux07fXgDCDXBNKYQDm8xAffvpKxc1d44iHBcXlRAgapeaxk
In the heavy rains that preceded Cyclone Idai, a broad swathe of southern Malawi was submerged by flood waters. At least 60 people have died, and tens of thousands were made homeless. But things could have been much, much worse. Understanding how affected communities took steps to protect themselves, sometimes long before the waters rose, is key to understanding how to mitigate the impact of extreme weather events in the future. In the stories of these villages lie the lessons that southern Africa must learn if it is to have any chance of coping with climate change.
By Simon Allison in Ndamera and Chikali
Part 1: Thaundi
With the luxury of hindsight, we know that Biasi was in the middle of the heavy storm that would leave much of southern Malawi underwater. The storm then headed out into the Indian Ocean, where it gathered energy, returning as Cyclone Idai to pulverise Beira and surrounding provinces in both Mozambique and Zimbabwe.
Edward Biasi has been Thaundi’s headman since 1978. He thinks the village is now too dangerous for people to inhabit.
Among Biasi’s many responsibilities is reacting to extreme weather warnings. Knowing how to respond is never easy. Evacuating means abandoning the maize and bean crops, which were weeks away from harvest, and this year was on track to be a good one. Without that food, the village cannot eat. It also means leaving livestock to their certain deaths.
Nonetheless, he made his decision quickly. Bitter experience has taught him the value of caution. It was time to pack up and go.
This is not the first time he has had to make such a difficult call. Biasi has been headman since 1978, when he took over from his grandfather. He cannot remember how many times Thaundi has had to be evacuated, but he does know that it is happening far more often than before. The last major flood in southern Malawi was just four years ago, in 2015, in which at least 176 people were killed. “In my village we always get flooded. But it’s different from the past. It would happen once every ten years, and the waters weren’t so high. Now it’s more frequent.”
After each disaster, with increasing reluctance, he returns home. “We keep going back because we can’t have land anywhere else.”
Five chiefs report to Biasi, and at around 10pm he spoke with them about the impending disaster. They did not have a formal, sit-down discussion - there simply wasn’t time. Preparations to leave began immediately, and by 8am the next morning the first canoes were crossing the river, heading to the relative safety of Ndamera, a larger village on higher ground on the other side of the river. Ndamera has for decades offered refuge when the waters come.
There was no room for people to bring much in the way of belongings - just the clothes on their backs and maybe a few pots and pans - and all the goats, chickens, and guinea fowl had to be left behind.
Not everybody heeded the call to evacuate. “Most left, but some stayed,” said Biasi. “Sometimes people are not sure, they think the water is not moving so fast. But this time they were wrong.”
Never a bluegum
In times of great calamity, the smallest details can be the difference between life and death. What saved Nessie and her family’s life was the knowledge that bluegum trees become slippery when wet. Mango trees, however, retain their grip.
After two days spent clinging to a mango tree, a fisherman arrived in a dugout canoe to rescue Nessie and her family.
She strapped her two-year-old daughter to her back with a fold of chitenge. Her husband took their seven-year-old son. They looked for a suitable mango tree - never a bluegum - and clambered up.
And then they waited, watching as the water rose until their house and all their belongings were totally submerged. For two long days and longer nights they waited, but no one came to their rescue. While she waited, Nessie could not stop thinking about what happened to another woman in her village, in the 2015 floods. This woman, also stuck in the high branches of a tree, collapsed with exhaustion and fell into the water below. Neither her nor her baby survived. Even now, with Nessie’s baby giggling safely on dry land, this is all she can think about. “I keep imagining what would happen if I fell into the water and what would happen then.”
She didn’t get much sleep on the tree. “There were times when I dozed off, but I would wake up every few minutes. We were so hungry. The baby was so hungry that she was biting my arm.” Eventually, a fisherman rowed up in a dugout canoe, searching for survivors. Rescue came at a price - 1000 Kwacha (R20) per person - but the family was in no position to bargain.
The fisherman rowed them to a makeshift port on the east bank of the river, where they waited for another two days with no blankets or mosquito nets, and only a few handfuls of food, until word came from their chief to join the rest of the village in Ndamera. “This time, it’s better than in 2015. This time no one from our village died,” said Nessie.
Even my laugh is weak
Joel Kadalinga, 47, saw trouble coming - years ago. After the 2015 floods, he saved up to build a house in Ndamera. “Our area is a flood and famine area. One year I got the money and I moved. It’s very safe here because it’s up.” Him and his family still live and farm in Thaundi. They grow maize to eat, and beans and sugar cane to sell. But at the first hint of floods to come, they escape to Ndamera, only a couple of hours away in normal times, to wait it out. This year they moved in January, just in case, and when the river began to rise in Thaundi they were already in a fully-equipped place of safety.
“It was hard for the village to sense that this was a dangerous situation,” he said. “The weather these days is unpredictable. It was only when the water was up to their necks that they moved.”
Months before the floods, Joel Kadalinga moved his family to another village at a higher elevation.
There is only so much anyone can do, however. Although all the new arrivals have some form of temporary accommodation and the children have been welcomed into the local school, food remains scarce. Rations provided by government and humanitarian agencies are just two cups of maize meal per family per day. For the rest of their diet, the men go out to hunt or fish or forage, or try to pick up piece work in unaffected communities. It is never enough. “I’m so hungry that even my laugh is weak,” said Nessie.
Kadalinga is even more worried about what happens when the flood waters recede, and the villagers of Thaundi return home. “Three months from now, we will go back. We will continue with our yearly activities. All the moisture in the soil means that the next harvest will be excellent, but we have to survive until then. We need support to do so.” And then? “We are worried. It’s tiresome. We build our homes and then two or three years later they are destroyed.”
For Biasi, the Thaundi headman, there is no small measure of pride that he made the right decision. Despite the devastation of their homes, no one from Thaundi died in the floods. No one was injured. But he knows, if the weather continues to behave so erratically, that there will be a next time. “I don’t think the village will still be there in 50 years. I don’t think anyone should live there now. But that’s the only land that we have, so what choice have we got? It’s very painful for me and my people, but we have no choice.”
Part 2: Chikali
In Chikali village, also on the west bank of the Shire River, very near the border with Mozambique, memories of the last great flood are fresh. It was only four years ago, in 2015, and ten people from the village were killed. Markson Beka remembers it well: the waters rose at night, and it was chaos as people ran around in panic, not knowing what to do or where to go.
This time, when the floods came, the village reacted totally differently. Despite 1799 households in Chikali and the surrounding area being affected, there were no casualties. Not one. “It’s because of the awareness we created. We told people to move in time. We had a plan,” said Beka.
Markson Beka’s Village Civil Protection Committee learnt from the mistakes made during the 2015 floods.
The committee learned from the mistakes made in 2015, and put in place procedures to prepare for the next disaster, and to mitigate its impact.
The first step was to train residents to recognise the warning signs. “When we see more ants, that is a sign that more rains are coming. When we have continuous days of rain, then we can expect a flood,” said Beka.
Next the committee created assembly points on higher ground, so that people would know exactly where to go when they sensed trouble. This is not an option for all villages, but Chikali is lucky in that it is relatively hilly, and some areas are safe from floods.
The committee toured around all the low-lying settlements to ensure that everyone knew what to do when disaster struck.
Before the floods, this plot, now entirely bare, was occupied by five or six houses.
The significance of the whistles cannot be overstated, he said. Not only does the whistle serve as an alarm bell, it also allowed committee members to easily direct nervous crowds to places of safety. Again, in an emergency, it is the smallest details that can make the difference between life and death.
Once the waters have gone, and things return to normal, Enelisi Wiseman intends to ask the chief for a house on higher ground
Enelisi Wiseman was among those affected. When the whistles sounded, her and her family knew what to do. “When the disaster happened we were in our village. We then moved into the primary school.” Several days later, the village headman allocated land for her and 114 other households to construct temporary accommodation while they wait for the flood waters to recede. The new accommodation is already being built: reed huts to replace the clay-brick houses.
Around the village, at least in the areas where the waters have receded, the ruins of the houses that were destroyed are obvious in the collapsed walls and the piles of tumbled-down bricks; and in the patches of bare earth where even foundation stones were ripped from the ground.
Brains Kamanula, a community health worker with Doctors Without Borders.
Food remains a problem, however. The area is accessible only by boat, which makes it hard for humanitarian organisations to get there. Everyone’s crops have been decimated by the storms and the floods, and what little is left is being strictly rationed.
It could be several months until Wiseman and her family return home. When they gets there she will have to start again from scratch. She knows that hers is not a sustainable lifestyle in the long-term, that something has to change. “We have a tentative solution that we have discussed amongst ourselves,” she said. “We are desperate so we will go back and build temporary houses and go and plant our crops. After we harvest, we will go and ask the chief if we can have some land somewhere higher up.” This time she escaped with her life, and she doesn’t want to have to do it again.
(Photographs: Simon Allison)
http://atavist.mg.co.za/the-malawian-villages-that-took-on-the-floods-and-survived?fbclid=IwAR1kLik0FdDfux07fXgDCDXBNKYQDm8xAffvpKxc1d44iHBcXlRAgapeaxk
Flooding in Malawi: “This time around, the destruction is more of houses and farm produce”
29 March 2019

The same weather system went on to become Cyclone Idai which struck Mozambique and Zimbabwe on 14-16 March, 2019, one of the worst tropical cyclones on record to hit southern Africa. Labana, who has worked for MSF for 20 years in Malawi, was also part of MSF’s response to severe flooding in the same area in 2008 and 2015.
His historical understanding and deep engagement with local partners and communities in southern Malawi are vital to MSF’s ongoing response.
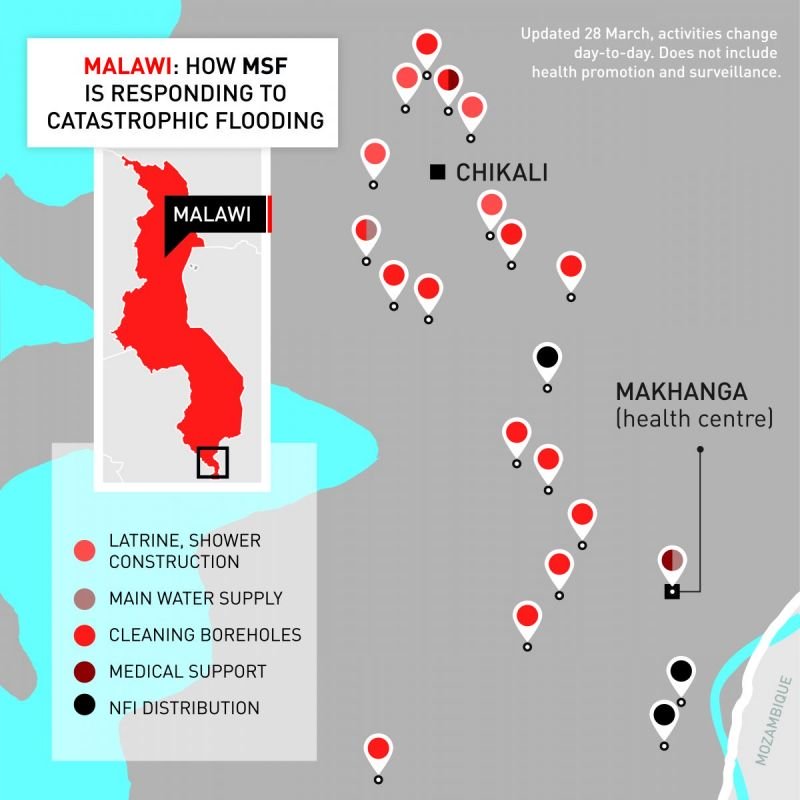
“Makhanga area, which is very fertile, is home to around 18,000 people who rear cattle and grow crops like maize and rice. It is low and flat and surrounded by the Shire River and its largest tributary, the Ruo, so it basically looks like an island,” says Labana.
“This makes it very prone to flooding. If there are rains in nearby Mulanje district or upstream in the City of Blantyre, and the Ruo swells, then the area is at risk. If there are rains upcountry and the Mwanza River swells, it can cause the Shire river to spill and the entire area is at risk. Heavy rains starting in early March affected all the southern districts, so the entire area has been largely submerged for weeks,” he says.
Donate towards MSF’s emergency response in Southern Africa
Learning from previous floods
The lessons Labana learned in responding to the previous severe flooding in Makhanga area in 2008 and 2015 are serving MSF’s current emergency response efforts. “In 2015 we mapped the most risky, flood-prone areas in order to focus our response, and identified people to work with closely in the community,” he says, adding that these relationships have enabled MSF to come in quickly, when the heavy rains were just starting, to assess the situation and plan an immediate response with the community, who already had some experience of how to distribute relief items.“In our previous flooding responses, we shared information on how to find and prioritise people who needed medical care. In 2015, a lot of people died in this area, but this year fewer lives have been lost to the flooding, partly because people now know where to find higher ground,” he says.
Makhanga health centre was severely flooded, but Labana says MSF experience of responding to previous floods again proved helpful. “In 2015, a lot of drugs were soaked in floodwater, ruining them. Afterwards, MSF raised the height of the shelves so that the drugs would be safe from the water, so this time the stocks were spared,” he says.
Shortages of food and clean water
Fewer lives have been lost in the 2019 floods but the damage caused to homes and crops has been immense. “It isn’t just crops that have been lost, it’s also food stored in homes in an area that was in need of food support even before it was flooded. The floods have contributed to great hunger already in the area,” says Labana.The flood waters have also submerged boreholes and destroyed toilets, and with thousands having to defecate in the open the risk of waterborne diseases such as diarrhoea and cholera breaking out is high. Labana says the area’s many swamps are breeding grounds for mosquitos, putting people at risk of contracting malaria. “People here are vulnerable in terms of their health right now, with many sleeping outdoors or in their chicken coops, because their homes were destroyed,” says Labana.
The borehole at Makhanga health centre was contaminated by the floodwaters but MSF staff have managed to clean it and ensure that the water is safer to use. Elsewhere, MSF’s water and sanitation teams have been distributing chlorine, cleaning water points, and constructing toilets and showers. “Our main concern is that we prevent an outbreak of diarrheal diseases and cholera,” Labana says.

Challenges getting medical care
The flooding in Makhanga has pushed most of the district’s health workers to higher ground in the north for safety reasons, leaving the few remaining health workers under severe pressure. “In the beginning, there was just one Ministry of health medical assistant and one hospital attendant. To support them, two MSF staff are providing basic healthcare, HIV services and disease surveillance, with approximately 150 consultations per day. We’re now seeing a lot of respiratory infections and malaria,” Labana says.Working with the Malawian District Health Office, the MSF medical team has done an outreach clinic to ensure access to primary health care services and to drugs for patients with chronic diseases, including HIV and tuberculosis, who lost their medications in the floods.
“MSF is providing healthcare, water and sanitation and distributing essential relief items and hygiene kits, but our wish is to see more organisations responding in areas that we cannot manage, such as food. Looking ahead, the community of Makhanga is really going to need more support,” says Labana.

To date, flooding has caused 59 deaths, 677 injuries, and the displacement of around 87,000 people in camps overall (OCHA, 22 March). One of the worst affected area is Makhanga area, which essentially remains an island cut off from all road access, though it has electricity again. While many thousands of people are currently sheltering in schools, churches and makeshift camps for displaced people, some are starting to return home to rebuild their houses.
There has been widespread destruction of agriculture and animals – an estimated 50 percent of the area’s crops may have been lost. An MSF team of 18 people is currently working with local authorities, communities and the health ministry to cover the needs of an estimated 18,000 people in Makhanga with health, sanitation and non-food-item supplies.
How Malawi saved lives in Cyclone Idai
Simon Allison
Africa Editor of the Mail & Guardian, based in Johannesburg, covering news and politics on the continent.
It was early March, and a towering, unrelenting storm had been battering the region for nearly a week. The storm eventually moved out to sea and gathered strength, making landfall again in southern Africa on 15 March as Cyclone Idai, before leaving a trail of destruction across Mozambique and Zimbabwe.
The storm submerged vast areas of southern Malawi, with the districts of Nsanje and Chikwawa hit especially hard. In total, an estimated 868,900 have been affected by the heavy rains and flooding, including 86,980 people who have been displaced and 672 injured. Some 60 deaths have been recorded.
The dramatically lower death toll, compared to past flooding events in Malawi, reflects lessons learned from floods in 2015 and meticulous preparations to mitigate the consequences of similar natural disasters – a preparedness that contrasts starkly with the difficulties humanitarian actors are experiencing in Mozambique and Zimbabwe in the wake of Cyclone Idai.
It is no accident Steven was among the first people contacted by residents. He has been a humanitarian worker for several decades, including 15 years with Médecins Sans Frontières. He is also from southern Malawi. One reason people knew to contact him was that they remembered meeting him during the last great floods in 2015 and had saved his number. At least 176 people died then.
“I want to emphasise the part of involving the community. It’s not good just to work through assumptions."
Listening to the locals
Steven believes other countries can learn from Malawi’s example.For MSF, one simple lesson from 2015 was to raise the height of the shelves where medication is stored, to prevent the drugs from getting wet.
According to Steven, an even more important lesson – as far as humanitarian organisations were concerned – was the importance of listening to and cooperating with local communities; of working with them to gain their trust, and then responding to their identified needs. For him, this is a process that began years ago.
“I want to emphasise the part of involving the community,” said Steven, who is still with MSF. “It’s not good just to work through assumptions, to say maybe they are traumatised, they don’t have anything, they don’t have money, they are illiterate. We can easily then miss the truth of the best way to help them.”
This approach had a direct impact on MSF’s emergency response this year.

It was also through these discussions – spearheaded by Steven – that MSF realised that local communities had already established emergency evacuation points, and so were able to direct mobile clinics to the areas with the greatest need. “Because of that, it was easier for us to help them [than in 2015]; it was faster,” said Steven.
While aid from external actors was better focused and made a difference, Steven believes the most effective response to Cyclone Idai came from within affected communities, whose members took extraordinary steps to minimise the scale of this year’s disaster.
Although preparations differed from village to village, examples included: creating village-level civil protection committees that took responsibility for preparations; establishing early warning systems that used whistles to sound the alarm; and identifying assembly points on high ground and informing people how to get there safely when the waters began to rise.
Fishermen to the rescue
The most effective homegrown response, however, may have been the enormous rescue operation mounted by local fishermen in dugout canoes. The fishermen ferried tens of thousands of people to dry land over the course of several days.One of those fishermen was a 32-year-old who gave his name only as Trouble.

Simon Allison/TNH
Trouble is a fisherman and watchman who rescued stranded families from tree tops and high roofs.
“I am one of them who was carrying the people,” he explained. “I would find them in the trees, or in rooftops. Most of them had no belongings.”
The people he found were hungry, injured, and traumatised. Some had been stuck in branches for days without food, he recounted.
“When the water came, we were only able to save our lives, not our belongings.”Trouble’s was not an entirely altruistic service. He charged 1,000 Kwacha ($1.37) per person if they could afford it. But if they couldn’t, he would take them anyway, he said.
Trading chickens for safety
Some fishermen struck a harder bargain.A woman who gave her name only as Maria said that when her village of Masanduko – a long swathe of cropland along the Shire River – became inundated, she sought refuge in a tree with her baby and five chickens.

Simon Allison/TNH
Maria's
village, Masanduko, was totally submerged by the floodwaters. She is
now living in temporary accommodation at Khungu Bwe Camp in Chikwawa
District.
Once on dry land, Maria knew to make her way to a temporary shelter in Khungu Bwe Camp, in Chikwawa District – one of 187 such camps in the country.
Khungu Bwe is one of the camps where UNICEF is helping those displaced by the disaster. The UN agency has built temporary toilets, decontaminated the water supply, and even set up a theatre troupe to educate people on health, hygiene, and sanitation.
When The New Humanitarian visited Khungu Bwe, actors – drawn from around the region and speaking in the local Chichewa dialect – were performing a skit that warned of the dangers of open defecation. The crowd of several hundred people roared with laughter.
“Usually we call this theatre for development,” UNICEF’s Ken Limwame, who is running the programme, said. “This time, it’s theatre for emergencies. This is a traumatised population, and this gives them some psychosocial help as well as conveying an important message.”
UNICEF, too, credited careful preparations with saving lives – preparations inspired by a desire to respond more effectively than in 2015.
The agency had stockpiled supplies in strategic locations in the flood-prone region, which meant it was able to respond much faster than in the past. As UNICEF spokesperson Rebecca Phwitiko put it: “The only thing that would have been better is to have even bigger stockpiles.”
(TOP PHOTO: Households escaped the floods mostly via dugout canoe, with whatever possessions they could salvage from the rising water. This canoe is pictured in flood waters near Bangula in Nsanje district.)
https://www.thenewhumanitarian.org/news-feature/2019/04/08/how-malawi-saved-lives-cyclone-idai?fbclid=IwAR0QOC-5b5VCQDrpPL-a5VqKOHHTdHitZPIIqQwV8TsmLskMRmb_ybkXc88
Subscribe to:
Posts (Atom)